What does the FDA do?
In the United States, medical devices are regulated by the Food and Drug Administration (FDA) to ensure their safety and efficacy before they are marketed and sold. When it comes to FDA regulation, two terms that are often used interchangeably are “FDA approved” and “FDA cleared.” However, there are key differences between these two terms that impact how medical devices are assessed and approved.
With new products and medical devices constantly being introduced into the market, it’s important to understand what the FDA regulates, the different classifications for regulation, and the primary differences between FDA-approved and FDA-cleared.
Understanding this information can help both patients and practitioners make informed decisions about the products and devices you choose to incorporate into your daily lifestyle.
What Does the FDA Regulate?

The FDA regulation process ensures that products are safe and effective for their intended use, with benefits that outweigh their potential risks. This regulatory procedure is crucial for protecting public health while simultaneously promoting innovation and competitiveness within the marketplace.
The FDA holds responsibility for regulating a variety of products, including:
- Prescription drugs
- Over-the-counter drugs
- Biologics (e.g., vaccines, blood products, biotechnology products)
- Products that give off radiation (e.g., X-rays, microwave ovens)
- Dietary supplements
- Medical devices
- Surgical implants
- Food additives
- Cosmetics
- Tobacco products
- Infant formula
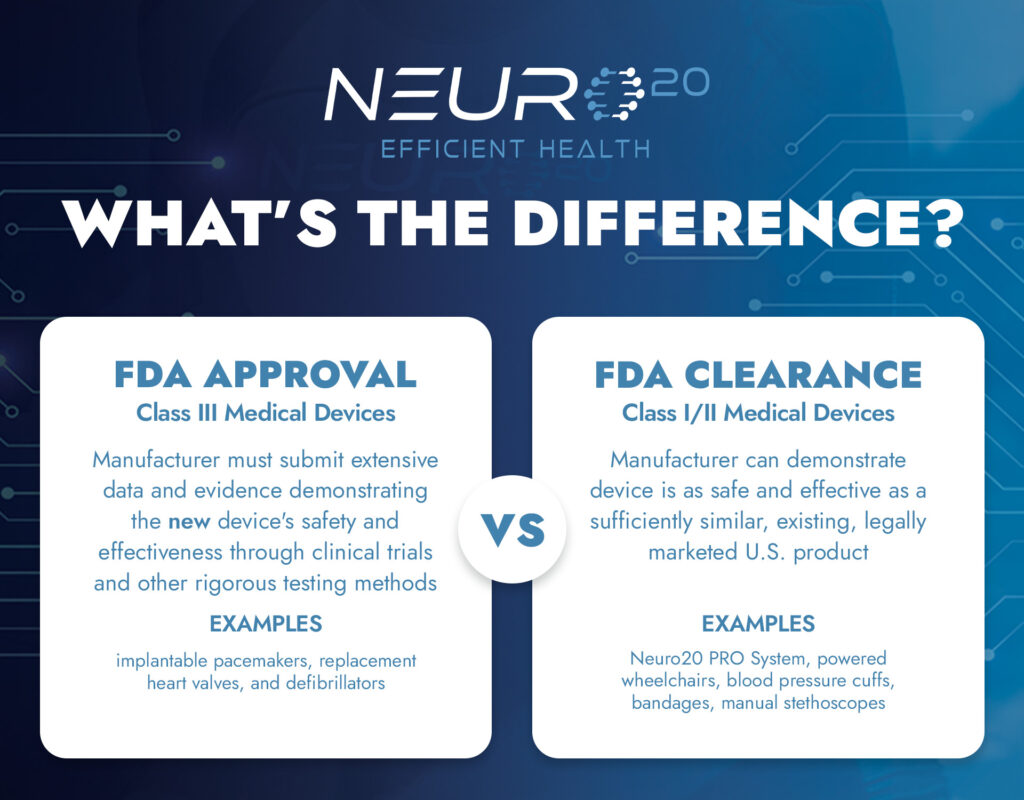
What is FDA Approval?
FDA approval is the regulatory process by which the FDA evaluates and approves a new medical device before it can be marketed and sold to the public. This approval process is reserved for high-risk devices, such as implantable devices or devices used for life-threatening conditions, that pose a significant risk to patient safety if they do not work as intended. To obtain FDA approval, medical device manufacturers must submit extensive data and evidence demonstrating the device’s safety and effectiveness through clinical trials and other rigorous testing methods. Once the FDA approves the data, the device can be marketed and sold to healthcare providers and patients.
What is FDA Clearance?
The FDA clearance process is typically reserved for lower-risk devices, such as diagnostic tools or medical equipment, that pose a lower risk to patient safety if they do not work as intended.
Unlike the FDA approval process, the FDA clearance process does not require clinical trials or extensive testing. Instead, medical device manufacturers must submit evidence that the device is “substantially equivalent” to an existing device already legally marketed in the United States. The FDA then reviews the evidence and determines whether the new device is safe and effective for its intended use. This is what the FDA has determined about the Neuro20 PRO System.
What Are the Different FDA Classifications?

Class I Medical Devices
Class I devices are considered low-risk and subject to the least amount of regulatory control. Examples of Class I medical devices include bandages, manual stethoscopes, and other devices that are not intended to be used for any invasive or potentially harmful procedures. These devices must adhere to general controls, such as registration with the FDA, appropriate manufacturing practices, and labeling requirements. Today, 47% of medical devices fall under this category and 95% of these are exempt from the regulatory process.

Class II Medical Devices
Class II devices are considered moderate-risk and require more regulatory control than those in Class I. Examples of Class II medical devices include the Neuro20 PRO System, TENS devices, powered wheelchairs, and blood pressure cuffs. These devices require special controls in addition to the general controls that apply to all medical devices, including post-market surveillance and patient registries. For most class II medical devices, a premarket notification is the chosen pathway to market. Also known as a 510(k), a premarket notification requires a product submission to the FDA that successfully demonstrates two claims:
- The proposed device is sufficiently similar to an existing and legally marketed U.S. product
- The proposed device is as safe and effective
as the predicate device
Currently, 43% of medical devices fall into the class II category.

Class III Medical Devices
Class III medical devices represent only 10% of the medical devices regulated by the FDA. Class III devices are considered high-risk and are subject to the most regulatory control. These devices usually sustain or support life, are implanted, or present a potentially unreasonable risk of illness or injury. Examples of Class III medical devices include implantable pacemakers, replacement heart valves, and defibrillators. These devices are subject to premarket approval, the most stringent level of FDA review. Premarket approval involves a comprehensive scientific review of the device’s safety and effectiveness, including clinical trials and detailed testing data. Class III devices require both general controls and special controls to ensure their safety and effectiveness.
Summary
The primary differences between FDA approval and FDA clearance are the level of regulatory scrutiny, the types of evidence required to demonstrate safety and effectiveness, and the types of devices that undergo each process. FDA approval is standard for higher-risk devices that pose a significant risk to patient safety (class III), while FDA clearance is typically reserved for lower-risk devices that are unlikely to cause harm if they do not work as intended (class I and class II).
Through two distinct regulatory procedures, both FDA approval and FDA clearance are critical processes that protect public health and safety. Whether a device undergoes approval or clearance, healthcare providers and patients can feel confident that the product or medical device they are using, such as the Neuro20 PRO System, has been evaluated by the FDA and is both safe and effective for its intended use.